Long COVID - neurological effects are more complex than just fatigue
i have 'chronic' mono since about 2002, confirmed by blood tests. there is chronic lymes, post polio syndrome.....its not that usual for a virus to have long term...even life long effects.
Lyme disease can totally suck and its variability gives the sufferer that extra special quality of not being believed. Borellia can really suck, plus ticks are also vectors for **** like viruses and parasites.
Speaking of mono, a report in Scientific American today gives some detail on how the Epstein Barr virus has been implicated in multiple sclerosis. This is another example of how even though the majority of humans carry the EBV, only a small percentage suffer the more major consequences.
https://www.scientificamerican.com/article/epstein-barr-virus-found-to-trigger-multiple-sclerosis/
The EBV report kinda rhymes with what we're learning about COVID. Perhaps we'll be learning a lot more about it, enough even to merit a new DSM diagnosis, what with all the neurocognitive complications.
This COVID pandemic's constellation of long-term sequelae is a new problem that will develop in the midst of social media, where scientific & clinical expertise run up against misinformation and political agendas. It sounds a bit too precious and dramatic when I say it in my head before posting this reply but many people have died needlessly and many more will suffer because of the propagation of fraudulent voices - so I'm doing it anyway.
so far, no indication of MS...I never had a spinal tap though..even with all my complicated symptoms, they don't point to MS--at least not yet.
I am not so much concerned about catching acute covid, but I am worried I will be at very high risk for long covid because of my medical history
A discussion of the higher rate of mental health concerns in people who have survived a COVID infection.
Information on the exhaustion long COVID patients report.
Post-infectious fatigue syndromes, of all sorts, have occurred all over the world for a very long time. As the founder of the original NJ Chronic Fatigue Syndrome Association 30 years ago, I'd given too many presentations and attended too many medical conferences to count. It's occurred in small self-limited epidemics in Royal Free Hospital (London) in 1955, and Iceland, and Australia, and Incline Village on Lake Tahoe, and Upstate NY on goat dairy farms. The list is lengthy. There are sporadic cases, where there are no clusters of patients. It's been linked to Epstein-Barr, Cytomegalovirus, HHV-6, Brucellosis, Q Fever, Ross River fever, and other infectious agents. Most, but not all, are viruses.
The primary feature of post-infectious fatigue syndromes, whatever the cause, is that they are chronic, lasting for periods of time that no one can predict, and they are not curable. The best that can be done is symptomatic relief (if one is lucky). Some people get over it, some people have temporary remissions which are totally unpredictable.
The common assumption has been that the person's immune system has not shut off after it's fought off the acute illness. It's still ramped up, and that's what is causing the chronic symptoms. This is a simplistic approach. No one has been able to define a single mechanism for this. The research results have been all over the map. That's why there are no blood tests to prove you have this. The human immune system is extraordinarily complex.
With the prospect of millions of cases of Long COVID, and the applications of billions of $$$ in research funds, maybe we'll finally get some answers.
That’s the most effective summary of the topic I’ve ever read, metaphysician.
And your comment about blood tests brings to mind an old Tracey Ullman (Francesca) episode, though I can’t find the relevant clip now.
The best I can do is to find reference to it ( no video clip) - in this article (keep in mind it was over 30 years ago):
https://www.nytimes.com/1990/03/04/arts/tv-view-tracey-ullman-queen-of-the-skitcom.html
dickf3 said:
That’s the most effective summary of the topic I’ve ever read, metaphysician.
And your comment about blood tests brings to mind an old Tracey Ullman (Francesca) episode, though I can’t find the relevant clip now.
Thank you. That was probably as terse as I could make it. In case I hadn’t made it clear above, it’s regarded as a syndrome, not a disease, because it’s a collection of signs and symptoms.
There have been so many dead-ends in the research. Nothing universal ever popped out. There was never enough money to pursue the intriguing anomalies that would occasionally show their faces. Now that there are so many new diagnostic approaches, perhaps we can hope for significant progress. Back when I was involved, genomics barely existed, proteomics hadn’t been invented. So many more lab techniques are now available and almost affordable, that extramural grants from the National Institutes of Health could have a very significant impact. It’ll be needed. The potential impact of severe disability from COVID could be enormous, far exceeding most other autoimmune diseases.
BTW, I’m a huge Tracey Ullman fan to this very day. Her Angela Merkel is fabulous, as are her sendups of the various Windsors.
Another report. This one is about heart problems post COVID.
https://www.npr.org/sections/health-shots/2022/02/21/1081810074/omicron-ba2-variant-spread
(Yes, i am a little lazy about reading medical reports.)
Peter, is there any information yet about whether the long-term effects are connected to the severity of the original illness? Just wondering whether the vaccinations seem to be helpful in that way too....
While the severity of an acute COVID infection correlates with the initial viral load, it is unclear regarding whether long-term COVID effects match up so well. This is one report indicating that people have these problems even though their acute case was mild.
This Nature review article is heavy duty and long! Right now I don't have time to unpack it.
https://www.nature.com/articles/s41591-020-01202-8
This is a short & general discussion on long COVID. It is the latest report I found after a quick search. It's from December 21, 2021.
https://www.rivm.nl/en/coronavirus-covid-19/long-covid
We do not know yet exactly why some people have long-term symptoms after a SARS-CoV-2 infection. There seems to be some correlation with higher ages and the symptoms that the person had in the first phase of the infection. People who were hospitalised for COVID-19 and people with an elevated BMI or asthma also appear to be more likely to have post-infection symptoms that persist for longer. However, even people who have not been hospitalised can experience persistent symptoms. Long COVID appears to occur more frequently in women. After a serious SARS-CoV-2 infection, patients sometimes still have decreased lung function for months after discharge from hospital, as well as lung abnormalities that can be observed on X-rays or lung scans.
PeterWick said:
Another report. This one is about heart problems post COVID.
https://www.npr.org/sections/health-shots/2022/02/21/1081810074/omicron-ba2-variant-spread
There have been a number of studies documenting the damage caused to multiple organs caused by widespread micro clots in patients with serious acute illness. This can lead to long term disability. It’s unclear, however, whether this plays a significant role in Long COVID.
I just perused the Nature article. Very heavy going and mostly above my paygrade, so I downloaded the pdf for rereading later.
One area I’ve seen little mention of: Studies of IgM antibody responses. While normally short lived, therefore tough to implement, there have been any number of instances of long term IgM antibody production in post-viral syndromes. This is always indicative of immune dysregulation, often resulting in unwarranted cytokine production. Anyone who’s ever had IL-2 infusion for treatment will tell of the profound fatigue that it induces. While there’s never been a consistent proof of a specific cytokine upregulation in a given syndrome, there have been all sorts of mixed cytokine upregulation. The immune system is so incredibly complex that consistency is rarely to be found.
Metaphysician, you might not be aware of the ‘newer’ non-IgE-mediated antibody/allergy reaction: the mast cell activation disorder, that results in massive inflammation and other classic allergy signs. I can even react allergically to loud noises, and to things that surprise me. I know there’s an IL connection but I can’t remember which, sorry.
My immunologist explained that MCAD is a step before IgE-mediated allergies; he believes if you can control the inflammation, you can prevent most of chronic conditions people currently live with. (Prof Peter Smith, Griffith Uni)
ETA: Metaphysician, I see that Prof Pete has published a paper on CFS (I did not expect the citation to come out this way - sorry!! The journal is Frontiers of Public Health, 8:420
TY - JOUR
AU - Close, Shara
AU - Marshall-Gradisnik, Sonya
AU - Byrnes, Joshua
AU - Smith, Peter
AU - Nghiem, Son
AU - Staines, Don
PY - 2020/08/01
SP - 420
N2 - Objectives: This study aims to estimate direct and indirect health economic costs associated with government and out-of-pocket (OOP) expenditure based on health care service utilization and lost income of participants and carers, as reported by Australian Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) patient survey participants. Design: A cost of illness study was conducted to estimate Australian cost data for individuals with a ME/CFS diagnosis as determined by the Canadian Consensus Criteria (CCC), International Consensus Criteria (ICC), and the 1994 CDC Criteria (Fukuda). Setting and participants: Survey participants identified from a research registry database provided self-report of expenditure associated with ME/CFS related healthcare across a 1-month timeframe between 2017 and 2019. Main outcome measures: ME/CFS related direct annual government health care costs, OOP health expenditure costs, indirect costs associated with lost income and health care service use patterns. Results: The mean annual cost of health care related expenditure and associated income loss among survey participants meeting diagnostic criteria for ME/CFS was estimated at $14.5 billion. For direct OOP and Government health care expenditure, high average costs were related to medical practitioner attendance, diagnostics, natural medicines, and device expenditure, with an average attendance of 10.6 referred attendances per annum and 12.1 GP visits per annum related specifically to managing ME/CFS. Conclusions: The economic impacts of ME/CFS in Australia are significant. Improved understanding of the illness pathology, diagnosis, and management, may reduce costs, improve patient prognosis and decrease the burden of ME/CFS in Australia.
T1 - The Economic Impacts of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in an Australian Cohort
VL - 8
DO - 10.3389/fpubh.2020.00420
JO - Frontiers in Public Health
ER -
Okay, the title is alarming but these preliminary findings are grabbing some attention. PET scans adapted to track the bodily locations where SARS-CoV-2 accumulates show that it infects cells in the male genitourinary tract. They are investigating how the virus could be causing the symptoms in male plumbing that had been attributed to things like inflammation.
https://news.northwestern.edu/stories/2022/03/covid-infects-penis-testicles-and-prostate/
Well, if that news doesn't drive a surge in vaccination rates, nothing will.
After all, hockey players wore cups long before it occurred to them to wear face protection.
The results are clear and very significant: Compared with similar people who had not been infected with SARS-CoV-2, those who recovered from infection had many more blood clots, heart problems and strokes. The extent of the differences across the 20 different cardiovascular conditions is among the greatest of any clinical study I have read. It is jaw-dropping.
These Covid-19 symptoms raise new questions - A CNN Opinion piece
https://www.cnn.com/2022/03/04/opinions/covid-19-cardiovascular-symptoms-sepkowitz/index.html
That paragraph above the link is from the article. They have had a long time to follow up on survivors of the 2020 version of SARS-CoV-2. These findings are from studying the longer-term consequences in survivors. Vascular tissues were affected and many people did not notice any such symptoms. Doctors didn't catch the pattern either until later. All the pulmonary trauma was overloading the medical response to it.
I have been telling people about the way more frequent blood clots cause random damage. Most of the cases eventually involve the heart, lungs, and brain and a blood clot is the worst of all lottery tickets to get. Each pattern of harm is different. That's one of the reasons they try to address blot clots elsewhere like the calf aggressively before they travel to more dangerous places. In the brain, I know how brain tissues respond to harmful things, especially toxins, from my earlier laboratory studies and now from my current work and it can be devastating. I hope you never have to experience a stroke, either from the survivor's standpoint or the caregiver's.
We know that the delta and omicron variants caused significant waves of their own and those variants behaved differently than the original (alpha) virus. It will take some time to characterize those variants' sequelae. Could be the same, could be easier to handle or they could be correlated with the overall average severity of each variant's effects. We just know that there are millions of people that are waiting to find out. I'm curious to see if the subsequent cardiovascular issues correlate with the viral load a patient had when they were infected. That would make sense but COVID has shown us it gives not a single **** about what would make sense. A mild infection (or even asymptomatic ones) might still make a person at a higher risk of the 20 cardiovascular problems they tracked in the follow-up monitoring. Omicron caused such a sharp increase in cases worldwide, particularly in America.
==================================
This is a memorable way of depicting what goes on every day in our blood vessels and helps one process just how much of a dang miracle it is that we live as long as we do.
"the very complicated dance of clotting and anti-clotting that goes on within each of our bodies every day."
Don't kid yourself. Getting COVID is best avoided and we'll be finding out why for years to come. Wear a mask if you're concerned and don't hassle others who do wear one.
https://www.nature.com/articles/s41591-022-01689-3 - This is the study cited in the CNN piece.
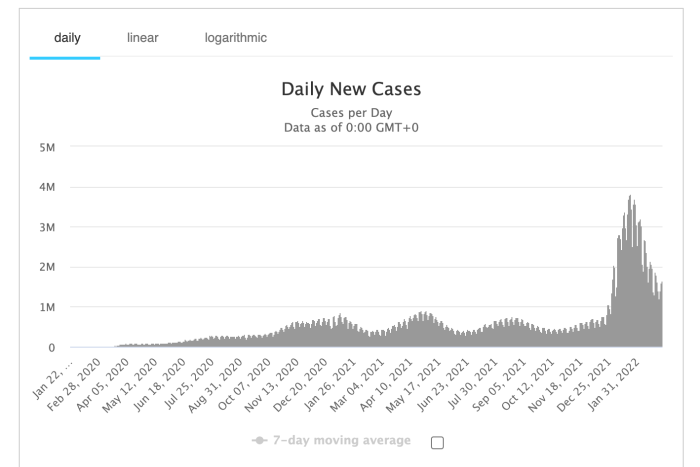
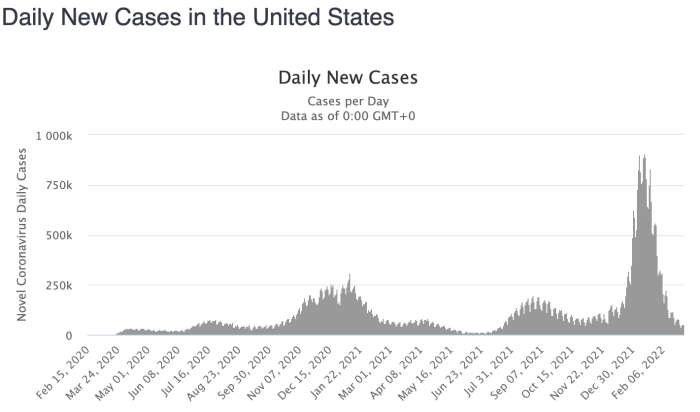
These two pics show just how much larger the delta and omicron waves were around the world and in the US. That report had figures that were shocking to the scientists conducting the study and those early cases aren't nearly as numerous as what is coming. I'm looking at chronic health conditions and the burden they're putting on the country's healthcare resources in one of my courses and those data are depressing as it is.
Without COVID, our demographics were already developing a large imbalance between the retiring workforce (and no longer paying into SS and other programs) and younger people joining it.
COVID's long-term health concerns may cause that imbalance to grow even wider much sooner, pushing a broader cross-section of the workforce into retirement due to medical conditions. That may also cause an increase in SSDI expenditure we're not ready for. Will they just make their approval process ratio even lower now? Being in the brain injury community has shown me some incredible stories of people getting rejected over and over when it is clear they cannot work. What will the coming increase in applications do? It may wind up causing some substantial policy changes and legislative work if the US is going to take care of its growing number of people in need of healthcare
Those cardiovascular problems cited in the CNN piece are almost all chronic conditions. Yes, they can be managed but the medical costs are likely to fall on the backs of consumers if the private insurance industry continues to operate in the interests of shareholders. How many of you have had your insurer somehow deny coverage for something? A certain medicine, test, or some procedure?
Public health is already a social justice concern. Non-white persons in the US suffered disproportionately higher morbidity & mortality due to COVID when I was doing contact tracing. It was absolutely clear when looking at the names and addresses in the case & contact databases of the different towns. Poorer people who could not afford to stay home and couldn't afford good protective masks are also the least equipped to handle chronic health conditions.
That Nature article is alarming, especially how the data showed milder infections still put people at risk of cardiovascular disease.
"Our analyses censoring participants at time of vaccination and controlling for vaccination as a time-varying covariate show that the increased risk of myocarditis and pericarditis reported in this study is significant in people who were not vaccinated ***** and is evident regardless of vaccination status."*****
Wear your mask if you're uncomfortable. Even if you're vaccinated. You don't want to get COVID. Ever.
Peter, on top of long covid symptoms, many people in our flooded areas are now being warned to watch out for mosquito-borne diseases especially Japanese encephalitis. When you compare signs and symptoms… *sigh* Of course, there’s a vaccine for the encephalitis but you need to be in an area with relatively decent roads, power, etc. and be willing to take it. 
Thanks for linking the article. Covid is a much nastier disease than just the acute illness that has already killed about a million Americans. I expect that physicians are already seeing patients with long-term health problems from covid and I would like to see if there are medical journals on this. I have already heard of people blaming the vaccine for long-term health problems, but these problems were very likely caused by a covid infection. Getting vaccinated is still our best defense. The somewhat rare side effects of the vaccine are far outweighed by the short and long-term ill effects of covid infection.
We have all heard about the stages of grief when we or a loved one gets a fatal diagnosis. First comes denial and then anger. Too many of our fellow Americans and also worldwide are still stuck in the denial or anger phase.
Are there any numbers and percentages. Is the chance of a vaccinated person getting long covid 1 in 10? 1 in 100? 1 in 1000? People have different risk thresholds. Pre-vaccine, I figured that if I caught covid, I would probably be okay, but the probability of a bad outcome was high enough that I was always careful. Now, I'm still respectful of masking requests, but I'm going out a lot more. While I certainly don't want to get infected, I don't feel particularly at risk any more.
Last week’s New Scientist looked at long covid in depth, and also cited many studies from around the world. I haven’t yet correlated them with those mentioned on MOL, but it might be worth checking with your library’s copy to see…@tjohn, if the subject is mentioned, I’ll drop back in and let you know.
Ya know, this is all I needed to do. I typed this into Brave and pressed Enter.
what percent of covid survivors get long covid?
The kinds of symptoms are like a cafeteria plan. They last for varying lengths of time post-COVID. They have different extents of severity. Some of the things I hear about are pretty strange. Like the sense of smell can disappear, but when it comes back there can be anomalies. One woman I know says it persistently smells like she's in a room with smokers. It has made it tough for her to eat sensibly. She's found it doesn't matter where she is, except that it is easiest to handle outside on a breezy day. It has been that way since she got her sense of smell back in August of 2020. A year and a half of that.
Things that long COVID causes.
This is from a year ago. That estimate is about 1/3.
https://www.webmd.com/lung/news/20210219/a-third-of-covid-survivors-have-long-haul-symptoms#1
This is from 6 months ago. The estimate is about half. That might be because they better understand things and can better sort out what are and what aren't COVID-sequelae.
https://www.sciencedaily.com/releases/2021/10/211013114112.htm
And finally, this link is from February of 2022. This article cites that the rate is around 10% percent.
https://health.ucdavis.edu/coronavirus/covid-19-information/covid-19-long-haulers
Maybe it's true what people say, and everybody is going to get it sooner or later. For myself, i'll take as much later as possible. Sounds a whole lot more risky than "flu," and that's leaving aside that i live with a person who already has chronic lung problems, and really needs to avoid the infection.
Thanks peter and joanne and all for info.
So, this is the sort of thing I was looking for.
https://www.webmd.com/lung/news/20211118/millions-worldwide-long-covid-study
Nov. 18, 2021 -- More than 40% of COVID-19 survivors across the world have or had long-term effects after recovering, according to a new study by researchers at the University of Michigan.
tjohn said:
So, this is the sort of thing I was looking for.
https://www.webmd.com/lung/news/20211118/millions-worldwide-long-covid-study
Nov. 18, 2021 -- More than 40% of COVID-19 survivors across the world have or had long-term effects after recovering, according to a new study by researchers at the University of Michigan.
Ahh, thanks for that link. Geez, that is a big number. Fatigue at 23% and dyspnea (difficulty breathing - I guess all the different ways are lumped there?) at 13% are the two big ones in that 40+%.
This is that study. It's a preprint so it hadn't been peer-reviewed as of November of 2021.
https://www.medrxiv.org/content/10.1101/2021.11.15.21266377v1
There's a new acronym that the medicos are going to try to get us to say.
Post-Acute Sequelae of COVID-19 (PASC)
Or maybe Long COVID or long haulers will still be the name people use.
Being an overweight older female with asthma and a thyroid issue who had a more severe COVID case was like winning the wrong type of raffle at the church fundraiser. Unfortunately, that demographic, especially minority women, is a more dismissed cohort when it comes to having their medical complaints taken seriously. That bias is still a problem for women presenting with any symptoms that could indicate a heart attack. If that 40% figure bears out there may be millions more cases of women presenting with these symptoms that get referred to as little old lady syndrome. Odd to see that Type II diabetes was not named specifically, just obesity. I had heard Type II DM all the time when people spoke of dangerous pre-existing conditions.
Here's the paragraph about prominent risk factors for PASC.
PASC risk factors
Although all included studies were screened for reported PASC risk factors, sex and pre-existing asthma were the only risk factors that were estimated in multiple studies and thus meta-analyzed. Female sex and pre-existing asthma had higher odds of having PASC with pooled estimated odds ratios (OR) of 1.57 (95% CI: 1.09, 2.26) and 2.15 (95% CI: 1.14, 4.05), respectively. Both meta-analyzed ORs were based on less than 5 studies and should thus be interpreted with caution. Among the studies that were not meta-analyzed, several found that individuals with more severe COVID-19 during the acute phase had higher risk of developing PASC.37,45,50,52 Additionally, two studies found older age to be associated with PASC.20,58 Other risk factors for PASC including number of symptoms during acute COVID-19,16 fatigue18, dyspnea,18,39 muscle pain,50 headache,18,20 myalgia,18 and pre-existing conditions such as obesity,18,52 comorbidity,45 and hypothyroidism37 were found positively associated with PASC (eTable 4).
SARS-CoV-2 is associated with changes in brain structure in UK Biobank
[I've separated out the 4 statements reporting the summarized findings.]
There is strong evidence for brain-related abnormalities in COVID-191–13. It remains unknown however whether the impact of SARS-CoV-2 infection can be detected in milder cases, and whether this can reveal possible mechanisms contributing to brain pathology. Here, we investigated brain changes in 785 UK Biobank participants (aged 51–81) imaged twice, including 401 cases who tested positive for infection with SARS-CoV-2 between their two scans, with 141 days on average separating their diagnosis and second scan, and 384 controls. The availability of pre-infection imaging data reduces the likelihood of pre-existing risk factors being misinterpreted as disease effects. We identified significant longitudinal effects when comparing the two groups, including:
(i) greater reduction in grey matter thickness and tissue-contrast in the orbitofrontal cortex and parahippocampal gyrus,
(ii) greater changes in markers of tissue damage in regions functionally-connected to the primary olfactory cortex, and
(iii) greater reduction in global brain size.
The infected participants also showed on average larger cognitive decline between the two timepoints. Importantly, these imaging and cognitive longitudinal effects were still seen after excluding the 15 cases who had been hospitalised.
These mainly limbic brain imaging results may be the in vivo hallmarks of a degenerative spread of the disease via olfactory pathways, of neuroinflammatory events, or of the loss of sensory input due to anosmia. Whether this deleterious impact can be partially reversed, or whether these effects will persist in the long term, remains to be investigated with additional follow up.
This was published on March 7, 2022 in the journal Nature. The link gets you to a page where you can delve into the reviewers' comments and other information.
Rentals
For Sale
Garage Sales
-
Multi Family Garage Sale Sale Date: Apr 20, 2024
More info














This became a topic in the spring of 2020 as people who recovered from the acute COVID infection found that they had a variable array of symptoms that lingered. Just what the hell it all means has been up for debate and sometimes flat-out denied.
This is a really long collective study on changes in the immune system in COVID survivors. There are limitations that the authors take care to mention (towards the end), true, but these are data taken from those who only had low-to-mid range COVID severity
https://www.nature.com/articles/s41590-021-01113-x
Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection
In summary, our data indicate an ongoing, sustained inflammatory response following even mild-to-moderate acute COVID-19, which is not found following prevalent coronavirus infection. The drivers of this activation require further investigation, but possibilities include persistence of antigen, autoimmunity driven by antigenic cross-reactivity or a reflection of damage repair. These observations describe an abnormal immune profile in patients with COVID-19 at extended time points after infection and provide clear support for the existence of a syndrome of LC.